In Clinical
Let’s get clinical. Follow the links below to find out more about the latest clinical insight in community pharmacy.Bookmark
Record learning outcomes
Learning objectives
After reading this learning update, you should be able to:
- Explain the causes of common upper GI conditions
- Advise patients on the most effective way to treat dyspepsia
- Be familiar with red flag warnings.
Upper gastrointestinal (GI) symptoms such as heartburn and indigestion (dyspepsia) are common. Although they can be related to serious underlying conditions such as peptic ulcer and cancer, they are much more often linked to milder conditions and can be relieved by lifestyle measures and OTC medication. However, community pharmacists should always be on the lookout for danger signs.
According to NICE Guideline CG184: “Pharmacists should offer initial and ongoing help for people with symptoms of dyspepsia. This includes advice about lifestyle changes, using OTC medication, help with prescribed drugs and advice about when to consult a GP.”
This feature will focus on the most common upper GI conditions, and the care that pharmacists and their teams can offer in terms of management, avoidance and when to refer.
Dyspepsia
‘Dyspepsia’ is not a diagnosis but a term used to describe a complex of upper GI symptoms including abdominal pain or discomfort, heartburn, acid reflux, and nausea and/or vomiting continuing for four weeks or longer.
NICE distinguishes “uninvestigated (or unidentified) dyspepsia” from diagnosed conditions such as gastro-oesophageal reflux disease (GORD), peptic ulceration or cancers of the oesophagus or stomach. Functional dyspepsia is where patients have all the symptoms but no physical abnormality is detected at endoscopy. These distinctions are useful in deciding on symptomatic treatment.
Causes of oesophagitis and peptic ulceration
Oesophagitis is commonly caused by repeated reflux of acidic gastric contents into the oesophagus. Unlike the stomach, the oesophageal mucosa has no protection against acid and is damaged by it, leading to inflammation and heartburn. Reflux of gastric contents is normally prevented by the lower oesophageal sphincter (LOSP), which operates like a one-way valve.
Reflux oesophagitis is associated with a weakened LOSP and is also more common with a hiatus hernia. Oesophagitis can also be caused by the irritant effects of medication (e.g. iron products; potassium chloride) or by radiation damage (e.g. following X-ray treatment).
Reflux oesophagitis symptoms can include globus sensation (the persistent sensation of a lump in the throat), regurgitation and sometimes wheezing or chronic cough at night due to regurgitated material ‘going down the wrong way’.
In some patients, chronic oesophageal reflux leads to pre-cancerous changes in cells lining the oesophagus, known as Barrett’s oesophagus. About one in 20 patients with Barrett’s oesophagus develop oesophageal cancer.
Peptic ulceration
Gastric parietal cells secrete acid but gastroduodenal lining cells also secrete mucus and bicarbonate that protect the epithelium from the damaging effects of gastric acid (and bile salts, pepsin, drugs, alcohol and Helicobacter pylori infection). Normally, the protective and damaging effects are held in balance but this can be disrupted, typically by H. pylori infection or NSAIDs.
H. pylori is able to penetrate the dense mucus layer that protects the gastric mucosa. It causes inflammation and worsens ulcers; it also appears to reduce duodenal bicarbonate secretion.
NSAID use is a common cause of peptic ulcer disease. These drugs disrupt the mucosal permeability barrier, leaving the mucosa vulnerable to injury. Up to 30 per cent of adults taking NSAIDs have GI adverse effects.
Risk factors for duodenal ulceration with NSAIDs include history of previous peptic ulcer disease, older age, female sex, high doses or combinations of NSAIDs, long-term NSAID use, concomitant use of anticoagulants and severe co-morbid illnesses. Physiological stress increases the risk of peptic ulceration.
More than 20 per cent of peptic ulcer patients have been found to have a family history of duodenal ulcers, compared with only 5 to 10 per cent in control groups.
Treatment
Most patients with dyspepsia prefer self-treatment and only seek medical advice if symptoms persist. Pharmacists can support patients to manage, treat and avoid dyspepsia/reflux symptoms. Key points for discussion with patients in line with current NICE guidance include:
- Review treatments (prescribed and OTC) to identify drugs that could be causing or exacerbating symptoms. Consider switching or discontinuing medication. In addition to NSAIDs and aspirin, other well-known candidates include bisphosphonates, calcium channel blockers, corticosteroids, iron preparations and potassium chloride
- Advise people to avoid known triggers where possible (e.g. smoking, alcohol, coffee, chocolate, tomatoes, fatty and spicy food)
- Raising the head of the bed on blocks (not using extra pillows, which simply ‘folds’ the torso and increases back-pressure on the LOSP) and having a main meal three to four hours before going to bed may help to relieve night-time reflux symptoms
- Offer advice on healthy eating, weight reduction and smoking cessation
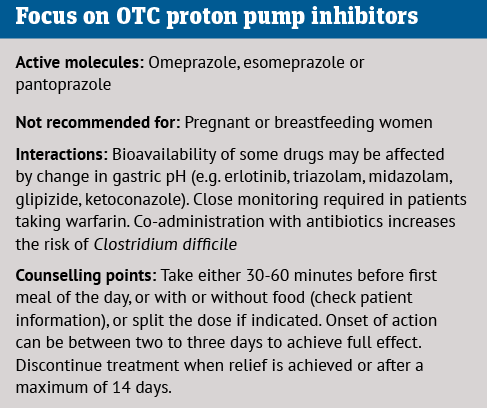
- Offer guidance on OTC medicines for self-treatment of heartburn and/or acid regurgitation, including antacids, H2 receptor antagonists (H2RAs) and proton pump inhibitors (PPIs). Antacids and H2RAs have a rapid onset of action, but the effects of H2RAs last longer. While the onset of action with PPIs is not rapid, the effects last significantly longer
- PPIs are the agents of choice for persistent, troublesome dyspepsia/reflux symptoms and offer effective, 24-hour acid suppression. Although early pharmacy-only PPIs were low-dose products, full-dose esomeprazole (20mg) and omeprazole (20mg) are now available as GSL items for short-term (up to 14 days) management of reflux symptoms
- Duration of acid inhibition with PPIs is 48 hours
- H2RAs (e.g. famotidine; nizatidine) have a rapid onset of action but less potent effects than PPIs. They are suitable for people with milder, intermittent symptoms
- Antacids have a rapid onset of action but the effects are short-lasting (limited by gastric emptying). Suitable for immediate symptomatic management and can be most effective when given one hour and three hours after food
- Alginate-containing antacids can be helpful for reflux symptoms. They form a viscous gel when in contact with acid and this sits on the surface of the gastric contents helping to reduce post-prandial acid reflux
- If possible, provide leaflets and/or signpost people for additional information/support
- Explain that if symptomatic measures do not provide adequate relief, referral for prescribed treatment will be the next step
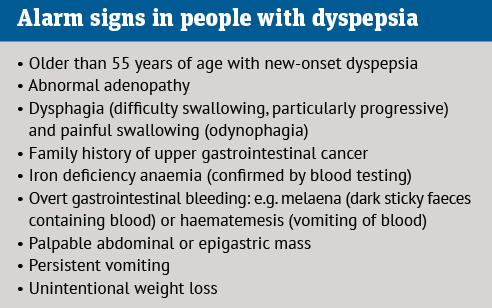
- Refer when necessary – immediately if red flags are present and if OTC treatments are ineffective or symptoms worsen.
First-line prescribed treatments for dyspepsia
- For dyspepsia without red flags, NICE advises empirical treatment with full-dose PPIs or ‘test and treat’ for H. pylori. Endoscopy is only necessary for patients with red flags or failure to respond to treatment. The prognosis is excellent
- If eradication treatment for H. pylori is indicated, then this will involve a seven-day course of triple therapy comprising a PPI twice-daily, amoxicillin 1g twice daily and either clarithromycin 500mg or metronidazole 400mg twice daily. For penicillin-allergic patients the treatment is a PPI, clarithromycin 500mg and metronidazole 400mg, all twice-daily. Good adherence is essential.
Helpful lifestyle advice
- Avoid foods that make symptoms worse, including rich, spicy, fatty and acidic foods, along with fizzy drinks
- Avoid bending, lifting or lying down straight after meals
- Lose weight if needed
- Cut down on caffeinated drinks, alcohol and smoking
- Do not eat for at least three hours before bed
- Prop up head and shoulders in bed
- Avoid medicines that can cause indigestion, such as calcium antagonists, nitrates, bisphosphonates, corticosteroids, NSAIDs, aspirin, iron, opiates, metformin, theophylline, anticholinergics and tricyclic antidepressants
Be alert for gastric cancer
Pharmacists should look out for the symptoms and risk factors that may herald the disease. By Mark Greener
Each year, doctors diagnose about 6,500 cases of gastric (stomach) cancer in the UK. While gastric cancer is not particularly common, especially compared with breast, prostate, lung and bowel malignancies, its prognosis is often dismal.
Cancer Research UK (CRUK) estimates that just 17 per cent of gastric cancer patients survive for at least a decade. About 4,200 people die from the malignancy annually – yet about half of cases are potentially preventable.
Globally, gastric cancer is the fifth most common cancer and the fourth leading cause of cancer death.1 The bacterium Helicobacter pylori, which colonises about half the world’s population, is responsible for much of the global burden. Most people infected with H. pylori develop chronic, asymptomatic inflammation. About 10 per cent experience peptic ulcer disease but 1-4 per cent develop gastric adenocarcinoma.2,3 (More than 90 per cent of gastric cancers are adenocarcinomas.1)
In the UK, H. pylori causes 41 per cent of gastric cancers, CRUK reports. H. pylori increases the risk of non-cardia stomach cancers (those not at or around the gastro-oesophageal junction) between three- and six-fold.3 Treating H. pylori infections with antibiotics reduces gastric cancer risk by as much as 47 per cent.3 Nevertheless, most people infected with H. pylori do not develop gastric cancer. To trigger carcinogenesis, H. pylori seems to interact with dietary and other lifestyle factors and the person’s genetic make-up.3
Preventing gastric cancer
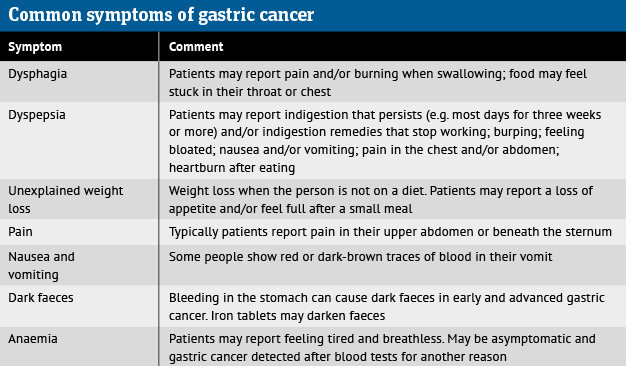
Early detection saves lives. CRUK estimates that 65 per cent of people in England diagnosed with stage 1 gastric cancer between 2013 and 2017 lived for five years – but five-year survival was just 25 per cent among people with stage 3 gastric cancer. Only about 20 per cent of people with stage 4 gastric cancer survived at least one year. Pharmacists should therefore refer any patients with symptoms (see table) to their GP.
According to CRUK, about half of gastric cancers develop in people aged 75 years or over. Between 1 and 3 per cent of gastric cancers seem to be hereditary.4 Nevertheless, 54 per cent of gastric cancers are potentially preventable, says the charity. Pharmacists can help patients address modifiable risk factors.
For example, patients with gastro-oesophageal reflux disease are prone to adenocarcinoma of the oesophagus and gastro-oesophageal junction. A Swedish study reported that recurrent symptomatic reflux increased the risk of oesophageal and gastro-oesophageal junction adenocarcinoma by 7.7 and 2.0 times respectively compared with controls free from reflux.
People with chronic, severe symptomatic reflux were 43.5 and 4.4 times more likely to develop adenocarcinoma of the oesophagus and gastro-oesophageal junction respectively.5
Pharmacists routinely offer lifestyle advice that can help reduce the risk of gastric cancer and several other malignancies and diseases by, for example, recommending limiting salt intake to help control blood pressure. CRUK reports that the risk of gastric cancer is 28-56 per cent higher in people with high intake of pickled foods and 68 per cent higher in those who consume large amounts of salt compared with low intake. Salt may exacerbate the carcinogenic effects of H. pylori infection.
Pharmacists are also involved increasingly in weight management and tackling addictions, which may also help prevent gastric cancer. Being overweight or obese seems to cause 6 per cent of gastric cancers. Heavy drinking (more than three units a day) seems to increase gastric cancer risk by 13-21 per cent, although disentangling alcohol’s effect from that of diet and smoking is difficult. Indeed, smoking causes 15 per cent of gastric cancers. CRUK also points out that being smoke-free could prevent 14 other types of cancer.
Gastric cancer does not capture the headlines like breast, prostate, lung and bowel malignancies – but half the cases could have been prevented and early diagnosis markedly improves survival.
For more on gastric cancer risk factors see cancerresearchuk.org.
References
1. Updates in Surgery 2023; 75:291-303
2. Clinical Microbiology Reviews 2010; 23:713-39
3. Cancers 2019; 11
4. Lancet 2016; 388:2654-2664
5. New England Journal of Medicine 1999; 340:825-31